What are root causes of hypothyroidism and thyroid dysfunction?
Hypothyroidism affects one in five women and one and 10 men.
The most common form of hypothyroidism is autoimmune driven Hashimoto’s thyroiditis where the body creates auto antibodies that attack self tissue.
The most common auto antibodies are anti-TPO, anti-TG, and anti-TSB.
Hypothyroidism can lead to:
- cold intolerance
- hair thinning/loss
- dry skin fatigue
- inability to concentrate
- elevated lipid markers
- weight loss resistance
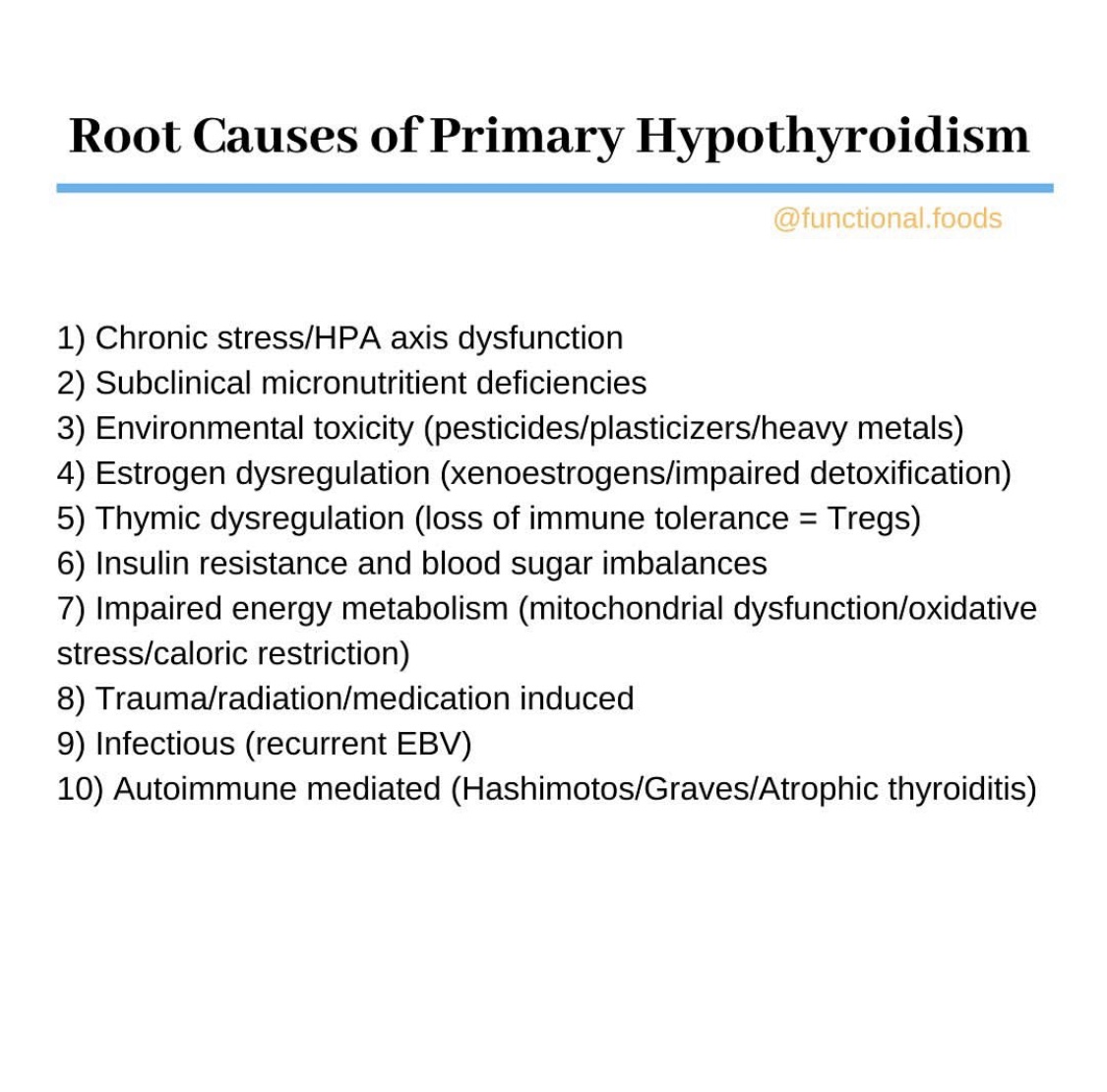
Root Causes for Thyroid Dysfunction:
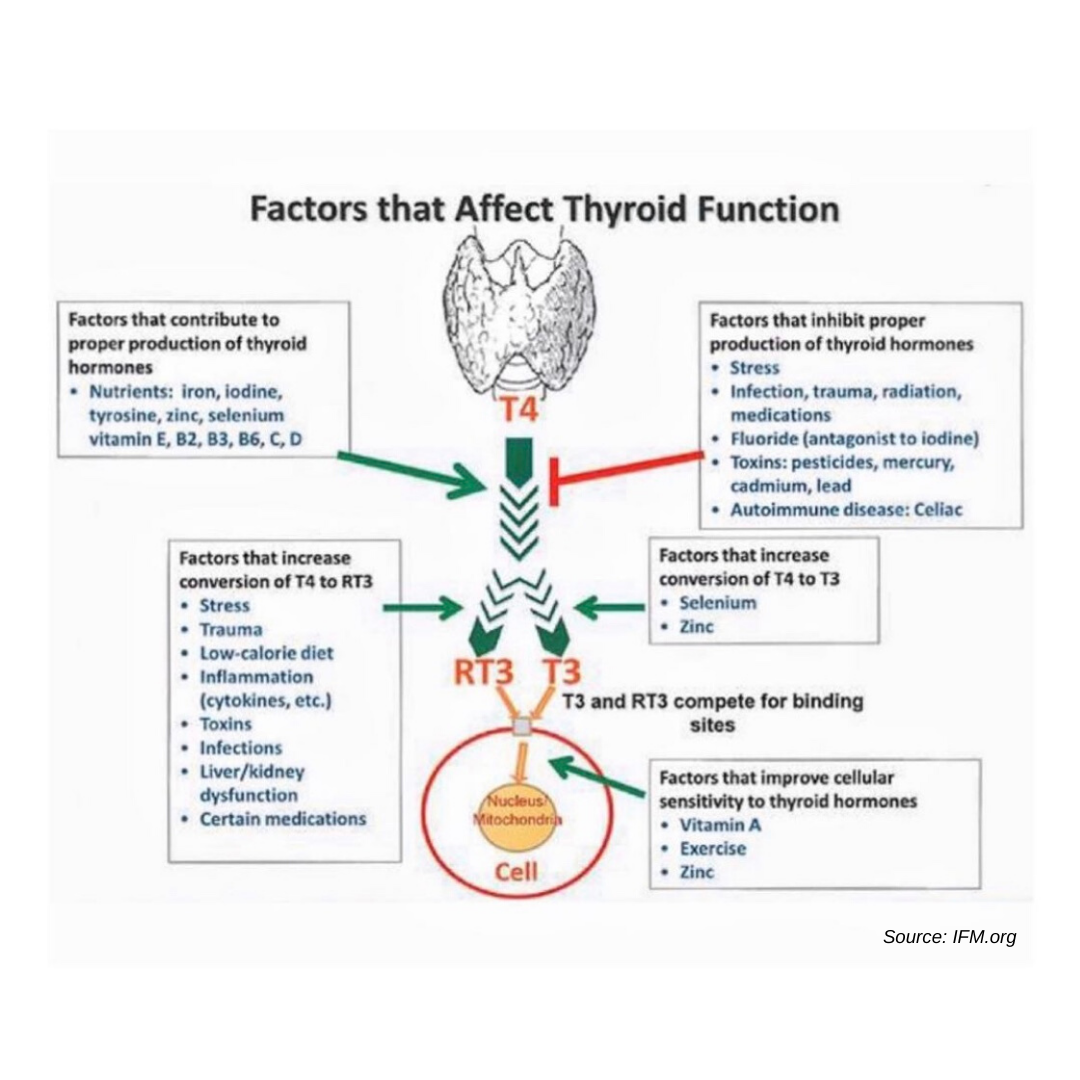
When it comes to proper thyroid function, it’s important to assess the bodily terrain and assess root cause factors that can be causing the thyroid to function suboptimally.
High estrogen levels can interfere with proper thyroid function by increasing thyroxine binding globulin (TBG) levels which decrease the amount of available active free T3 hormone. This happens in pregnancy as well.
Iodine is necessary to make thyroid hormone and helps maintain estrogen balance. Therefore, low iodine levels can exacerbate high estrogen levels. The phytoestrogens in soy can also worsen hypothyroidism in the context of iodine deficiency.
High cortisol secretion in response to stress blocks the pituitary gland from making TSH and favors the conversion of inactive T4 to reverse T3, thereby rendering thyroid hormone useless.
Over time, chronically high cortisol can lead to depletion of DHEA, which is necessary for efficient conversion of T4 to active T3 hormone. Low DHEA is also tied to insulin resistance.
Low-calorie diets and prolonged fasting can interfere with thyroid function. This is more common in women than in men.
Heavy metals such as lead, cadmium, and mercury, can inhibit proper conversion of T4 to active T3. Fluoride, bromine, and chlorine, all of which are halogens found in our municipal water supply, competitively compete with iodine absorption.
Subclinical micronutrient deficiencies in iron, zinc, selenium, vitamin D, vitamin A, iodine, and several B vitamins are necessary for proper thyroid function and to improve cellular sensitivity to thyroid hormone.
Viral infections and chronic inflammation can contribute to excessive oxidative stress which impairs mitochondrial function and energy metabolism. Mitochondria can be supported by things like acetyl-L-carnitine, a-lipoic acid, ribose, NAD, and CoQ10.
Certain medications can also suppress thyroid function such as narcotics, corticosteroids, beta-blockers, and amiodarone.
There is a link between celiac disease and thyroid disorders. This is why many people with autoimmune thyroid disorders experience significant improvements in thyroid function on a gluten-free diet.
Most doctors will screen with TSH, but you might have to dig deeper and do a full thyroid panel that assesses fT4, fT3, rT3, anti-TPO, anti-TG.
SOURCES:
Brent G. Environmental Exposures & Autoimmune Thyroid Disease. Thyroid, 2010;20(7).
Collins A, et. al, Prevalence of vitamin B12 deficiency among patients with thyroid dysfunction. Asia Pac J Clin Nutr. 2016;25(2):221-226.
Holtorf K. Peripheral Thyroid Hormone Conversion and Its Impact on TSH and Metabolic Activity. Journal of Restorative Medicine. 2014;3(1):30-52. doi:10.14200/jrm.2014.3.0103.
Laurberg P, et. al. Prevention of autoimmune hypothyroidism by modifying iodine intake and the use of tobacco and alcohol is manoeuvering between Scylla and Charybdis. Hormones, 2013;12(1):30-38.
Mancini A, et. al, Thyroid hormones, oxidative stress, and inflammation. Mediators of Inflammation, 2016.
Mazokopakis EE, et. al, Is vitamin D related to pathogenesis and treatment of Hashimoto’s thyroiditis? Hell J Nucl Med. 2015 Sep-Dec;18(3):222-7.
Pirola I, et. al. Selenium supplementation could restore euthyroidism in sublinical hypothyroid patients with autoimmune thyroiditis. Endo Polska, 2016;67(6).
Sun X., et. al, Increased incidence of thyroid disease in patients with celiac disease: a systematic review and meta-analysis. PLoS One. 2016;11(12).
Van Zuuren, EJ, et. al. Selenium Supplementation for Hashimoto’s Thyroiditis: Summary of a Cochrane Systemic Review. Eur Thyroid J 2014;3:25-31.



